Discover how Clomid 50mg can offer a range of benefits for men, from boosting testosterone levels to improving fertility.
Clomid 50mg is a medication that is commonly used in the treatment of infertility in women. However, its benefits are not limited to just women. Clomid 50mg can also offer several advantages for men, particularly in the area of improving reproductive health. In this article, we will explore the various benefits that Clomid 50mg can provide for men.
Understanding Clomid 50mg

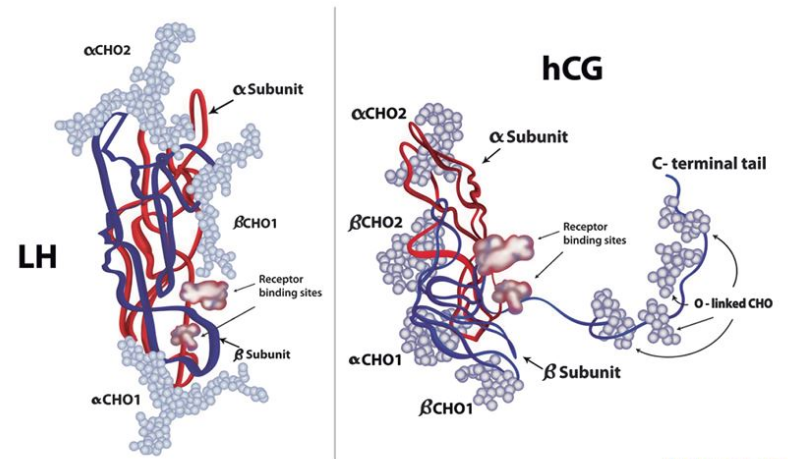
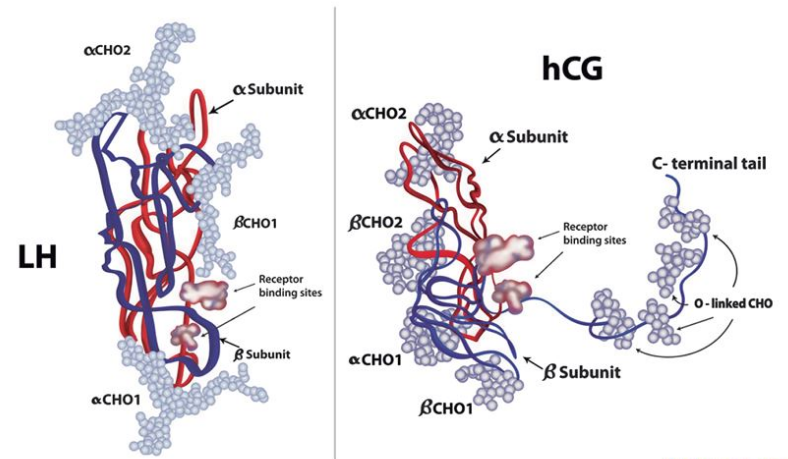
Before delving into the benefits of Clomid 50mg for men, it is important to have a basic understanding of what this medication is and how it works. Clomid 50mg, also known as clomiphene citrate, is a selective estrogen receptor modulator (SERM). It works by blocking estrogen receptors in the hypothalamus, which triggers the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones are crucial in stimulating the testes to produce testosterone.
What is Clomid 50mg?
Clomid 50mg is a well-known and widely prescribed medication used in the field of reproductive medicine. It is primarily used to induce ovulation in women, but it can also have significant benefits for men. Its active ingredient, clomiphene citrate, acts as an anti-estrogen, promoting the release of hormones that stimulate the production of testosterone.
How Does Clomid 50mg Work?
Clomid 50mg works by blocking the effect of estrogen on the hypothalamus, causing an increase in the production of LH and FSH. These hormones, in turn, stimulate the production of testosterone in the testes. By boosting testosterone levels, Clomid 50mg can help men who have low or suboptimal testosterone levels to increase their hormone levels and improve various aspects of their health.
It is important to note that Clomid 50mg should only be taken under the supervision of a healthcare provider, as improper use can lead to potential side effects. Common side effects of Clomid 50mg in men may include hot flashes, mood swings, and temporary visual symptoms. It is crucial to discuss any concerns or potential side effects with a healthcare provider before starting Clomid 50mg.
Potential Benefits for Men
Aside from its primary use in treating infertility in women, Clomid 50mg has shown promising results in improving testosterone levels in men with hypogonadism. Hypogonadism is a condition where the body does not produce enough testosterone, leading to various symptoms such as fatigue, decreased libido, and muscle loss. By stimulating the production of testosterone, Clomid 50mg can help alleviate these symptoms and improve overall quality of life for men with hypogonadism.
The Role of Clomid 50mg in Men’s Health
Clomid 50mg can play a vital role in men’s overall health and well-being, particularly in the following areas:
Clomid 50mg and Testosterone Levels
One of the primary benefits of Clomid 50mg for men is its ability to increase testosterone levels. Testosterone is a crucial hormone that plays a vital role in the development and maintenance of male reproductive organs and secondary sexual characteristics. Low testosterone levels can lead to a variety of symptoms, including decreased libido, erectile dysfunction, fatigue, and decreased muscle mass. By stimulating the production of testosterone, Clomid 50mg can help alleviate these symptoms and improve overall quality of life for men.
Clomid 50mg and Fertility
In addition to its role in boosting testosterone levels, Clomid 50mg can also have a positive impact on male fertility. Infertility is a complex issue that can have multiple underlying causes, including low sperm count and poor sperm motility. Clomid 50mg can help address these issues by increasing LH and FSH production, which stimulates the testes to produce more sperm. This can significantly improve sperm quality and increase the chances of successful conception.
Furthermore, Clomid 50mg is often prescribed off-label for men who are experiencing hypogonadism, a condition where the body doesn’t produce enough testosterone. Hypogonadism can result in a range of symptoms such as decreased bone density, increased body fat, and mood changes. By using Clomid 50mg to boost testosterone levels, men with hypogonadism can experience improvements in these areas, leading to a better quality of life.
Clomid 50mg and Athletic Performance
Another lesser-known benefit of Clomid 50mg for men is its potential to enhance athletic performance. Testosterone plays a crucial role in muscle development and strength, making it a key hormone for athletes looking to improve their performance. By increasing testosterone levels, Clomid 50mg can help athletes build lean muscle mass, recover faster from intense workouts, and enhance their overall physical performance. This has led some athletes to misuse Clomid 50mg as a performance-enhancing drug, despite its potential side effects and risks.
The Benefits of Clomid 50mg for Men
Aside from its impact on reproductive health, Clomid 50mg can also offer several other benefits for men:
Physical Benefits of Clomid 50mg
One of the physical benefits of Clomid 50mg is its potential to improve body composition and athletic performance. Testosterone is closely linked to muscle mass and strength, and higher levels of testosterone often result in increased muscle mass and improved athletic performance. By restoring testosterone levels to a healthy range, Clomid 50mg may help men build lean muscle mass, increase strength, and enhance overall physical performance.
Furthermore, Clomid 50mg has been found to aid in weight loss by promoting fat loss and preserving muscle mass. This dual action can be particularly beneficial for men looking to improve their body composition and achieve a leaner physique. By boosting metabolism and promoting the utilization of stored fat for energy, Clomid 50mg can support weight management goals.
Psychological Benefits of Clomid 50mg
Low testosterone can have a significant impact on mood and overall psychological well-being. Symptoms such as depression, irritability, and decreased motivation are often associated with low testosterone levels. By increasing testosterone production, Clomid 50mg can help alleviate these symptoms and improve mood, energy levels, and overall mental well-being.
Moreover, research suggests that Clomid 50mg may also have cognitive benefits for men. Improved testosterone levels have been linked to enhanced cognitive function, including better memory, focus, and overall cognitive performance. By supporting optimal testosterone levels, Clomid 50mg may contribute to improved cognitive abilities and mental clarity.
Potential Side Effects of Clomid 50mg in Men
While the benefits of Clomid 50mg for men are significant, it is important to note that there may be potential side effects associated with its use. It is essential to work closely with a healthcare provider to monitor and manage any potential side effects. Some common side effects of Clomid 50mg in men may include:
Clomid, also known as clomiphene citrate, is a medication commonly used in the treatment of male infertility. It works by stimulating the production of hormones that play a crucial role in sperm production. While Clomid is generally well-tolerated, some men may experience side effects during treatment.
Common Side Effects
- Hot flashes: Some men may experience sudden feelings of warmth, sweating, and flushing of the skin while taking Clomid.
- Mood swings: Changes in mood, such as irritability or emotional sensitivity, can occur as a side effect of Clomid in men.
- Nausea: Some individuals may experience feelings of queasiness or stomach discomfort while on Clomid.
- Headaches: Headaches are a potential side effect that some men may experience while using Clomid.
Rare Side Effects
- Visual disturbances: In rare cases, Clomid may cause visual changes or disturbances, such as blurred vision or sensitivity to light.
- Allergic reactions: Although uncommon, some men may experience allergic reactions to Clomid, which can manifest as rash, itching, or swelling.
- Enlargement of the testicles: Swelling or enlargement of the testicles is a rare but possible side effect of Clomid use in men.
- Decreased sperm production: While Clomid is intended to improve sperm production, in some cases, it may paradoxically lead to a temporary decrease in sperm count.
Precautions and Considerations for Clomid 50mg Use
While Clomid 50mg can offer several benefits for men, it is essential to exercise caution and consider certain factors before starting this medication. Consulting with a doctor is crucial to determine whether Clomid 50mg is the right choice for you. Some important considerations include:
When to Consult a Doctor
It is important to consult a doctor before starting Clomid 50mg to ensure that this medication is suitable for your specific situation. A healthcare provider can evaluate your medical history, conduct necessary tests, and determine whether Clomid 50mg is appropriate for you.
Dosage and Administration Guidelines
Clomid 50mg should only be taken under the guidance of a healthcare professional. The dosage and administration guidelines will vary depending on individual circumstances. It is important to follow the prescribed dosage and schedule to optimize the benefits and minimize the risk of side effects.
Before initiating Clomid 50mg treatment, it is crucial to discuss any existing medical conditions or medications you are currently taking with your healthcare provider. Certain medical conditions or drug interactions may affect the suitability of Clomid 50mg for your situation. Additionally, your doctor may recommend specific lifestyle changes or monitoring protocols while on Clomid 50mg to ensure the best possible outcomes.
Monitoring and follow-up appointments are essential aspects of Clomid 50mg therapy. Your healthcare provider may schedule regular visits to assess your response to the medication, monitor any potential side effects, and make any necessary adjustments to your treatment plan. These appointments are vital for ensuring the safe and effective use of Clomid 50mg in improving your health and well-being.